195,00 € – 695,00 €
Product details
Synonyms = Breast carcinoma-associated antigen DF3, CA15-3, Carcinoma- associated mucin Episialin, Epithelial Membrane Antigen (EMA), H23AG, KL-6, MAM6, MUC-1, MUC-1/SEC, MUC-1/X, MUC1- alpha, MUC1-beta, MUC1-CT, MUC1-NT, MUC1/ZD, Mucin 1 cell surface associated, Mucin-1 subunit beta, Peanut-reactive urinary mucin, PEM, PEMT, Polymorphic epithelial mucin, PUM, Tumor-associated epithelial membrane antigen
Antibody type = Recombinant Rabbit monoclonal / IgG
Clone = MSVA-672R
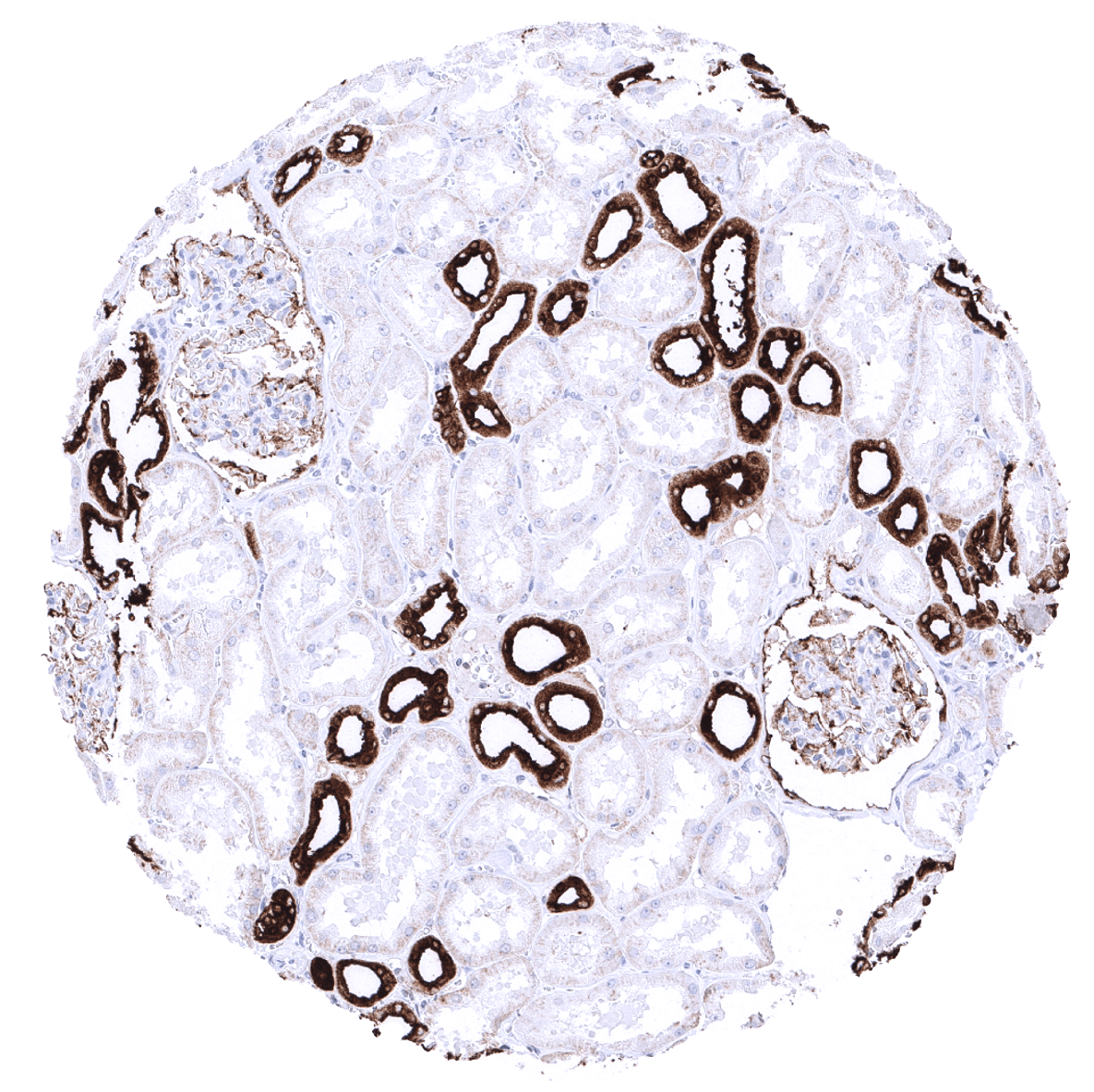
Positive control = Kidney: Distal tubuli and collecting ducts must show a strong cytoplasmic MUC1 staining while the staining should be at least moderate in the parietal and visceral sheets of the Bowman’s capsule and largely absent in proximal tubuli.
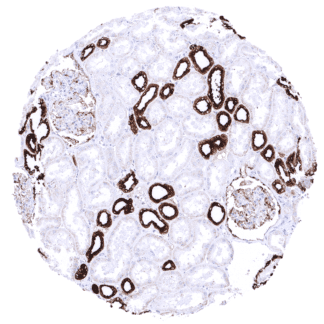
Negative control = Colon: MUC1 staining should be very weak or absent in colonic epithelium.
Cellular localization = Cytoplasmic & Cell Surface
Reactivity = Human
Application = Immunohistochemistry
Dilution = 1:100
Intended Use = Research Use Only
Relevance of Antibody
Biology Behind
Epithelial membrane antigen (EMA), also called Mucin 1 (MUC1), is a glycoprotein encoded by the MUC1 gene at 1q21. The protein is attached to the apical cell membrane of a large number of different epithelial cell types by a transmembrane domain. MUC1 is characterized by extensive glycosylation of its extracellular domain. If maximally glycosylated, MUC1 reaches a protein mass of up to 500 kDa and extends 200-500 nm beyond the cell surface. As other mucins, MUC1 lines the apical surface of various epithelial cells in order to protect these from infection by preventing the pathogen from reaching the cell surface. MUC1 also contains a cleavage site for sheddase induced release of the large extracellular domain. The protein also plays a role in cell signaling. In the cell nucleus, the protein MUC1 regulates the activity of transcription factors. Cancer studies have suggested a role of MUC1 in preventing cell death and promoting tumor invasion. Overexpression, aberrant intracellular localization, and changes in glycosylation of MUC1 can occur in carcinomas.
Staining Pattern in Normal Tissues
A variable, mostly moderate MUC1 immunostaining occurs in non-keratinizing squamous epithelia of all origins and in urothelium, with the staining often being more prominent in the upper than in the basal cell layers. A strong staining is seen in sebaceous glands while MUC1 is mostly negative or very weak in keratinizing squamous epithelium of the skin. A fraction of cells of tonsil crypts (moderate to strong) and some elements of Hassall’s corpuscles (weak to moderate) show a variable MUC1 staining.
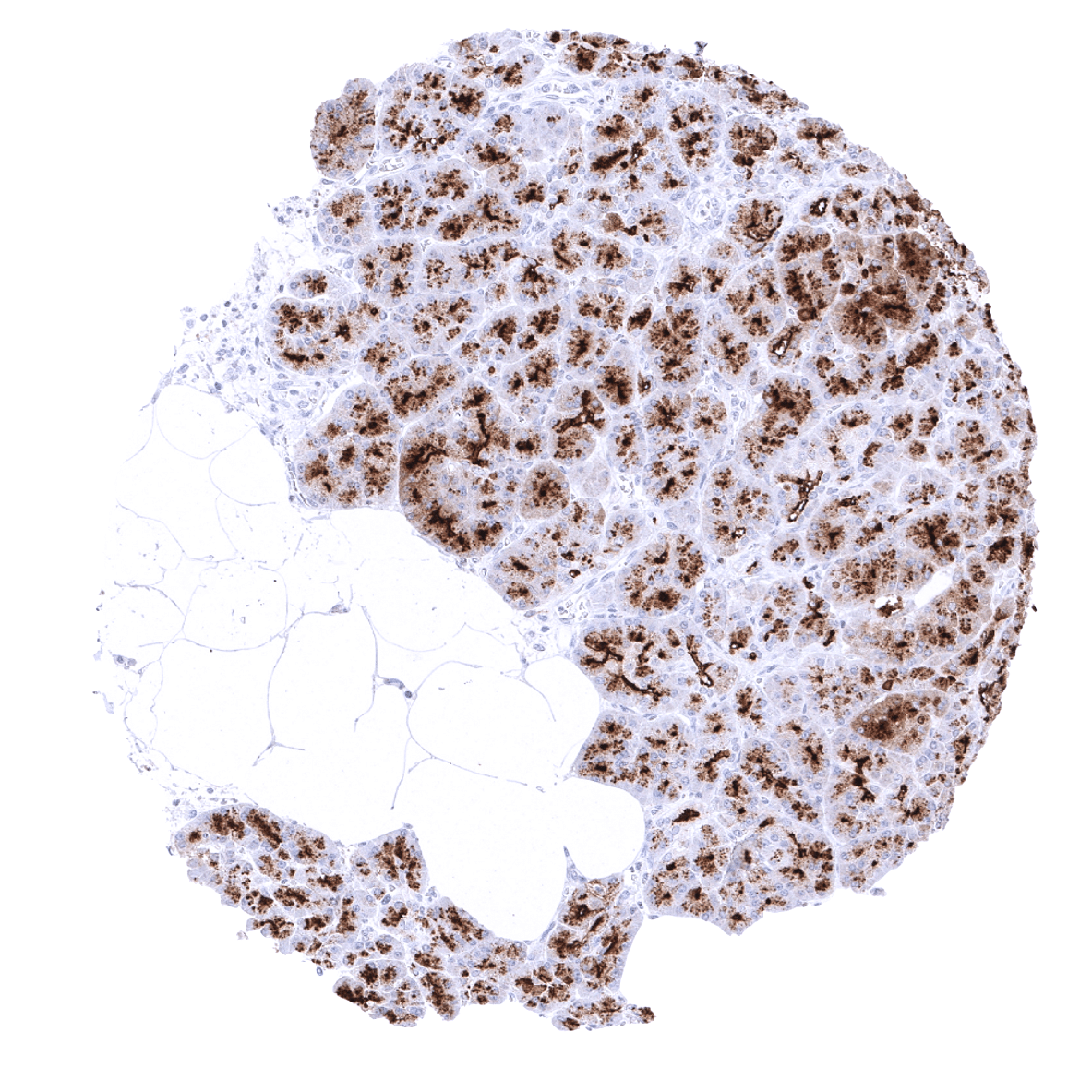
Mucus producing glands of the stomach show strong positivity while the remaining epithelial cells of the gastrointestinal tract including, duodenum, ileum, appendix, colorectum are MUC1 negative. A weak to moderate membranous staining is seen in gallbladder epithelium, pancreatic excretory ducts and intrahepatic bile ducts (predominantly apical), while hepatocytes are negative. Pancreatic acinar cells show a strong staining of the apical membranes and of granular (Golgi like) structures below the apical surface. Weak positivity of some pancreatic islets may represent contamination derived from adjacent acinar cells. In salivary glands, a moderate staining of apical membranes of serous cells and of excretory ducts is seen. Myoepithelial cells can be weakly positive. Rarely, apical membranes of some mucinous glands also stain. A weak apical membranous staining is occasionally seen in Brunner glands.
In the kidney, distal tubuli and collecting ducts show a strong cytoplasmic MUC1 staining while proximal tubuli are completely negative and both the parietal and visceral sheets of the Bowman’s capsule show weak to moderate positivity. Prostate shows a variable pattern with some glands (luminal and/or basal cells) strongly stained while others are completely negative. In the epididymis, the staining varies from diffuse cytoplasmic with apical predominance to apical membranous staining only. Focal apical staining occurs in seminal vesicle epithelium.
Fallopian tube, endometrium (stroma sometimes also positive), and the endocervix exhibit a strong cytoplasmic staining with apical predominance. In the placenta, a strong cytoplasmic staining occurs in amnion and chorion cells, while trophoblastic cells show a variable staining that varies between samples. The syncytiotrophoblast often shows a strong MUC1 positivity at the surface membrane. This phenomenon can also be limited to a few cells or groups of cells. In the first trimenon, the surface membrane of the cytotrophoblast can also show positive staining. In the breast, luminal cells show a moderate to strong cytoplasmic stain (apical predominance) while staining is often less intense in basal cells.
In the lung, a strong MUC1 staining is seen in pneumocytes and a moderate staining occurs in respiratory epithelium. Occasional weak MUC1 staining can be seen in bronchial glands. In the thyroid, a moderate apical staining is seen in follicles, sometimes accompanied by a moderate to strong cytoplasmic staining. The adenohypophysis shows a strong, predominantly apical staining in some gland-like structures. A faint staining of basal membranes may occur in the adrenal gland. In the adenohypophysis a moderate staining with apical predominance is seen in a fraction of cells/acini. Some cells in the germinal centres and plasma cells stain positive in lymph nodes. Sheaths of peripheral nerves show moderate MUC1 staining. In the brain, a variable fibrillar staining may be seen in samples from the cerebrum. A strong fibrillar staining occurs in the neurohypophysis.
MUC1 staining is absent in the parathyroid gland, follicular cysts in ovary, decidua cells in pregnancy, testis, and mesenchymal cells.
These findings are largely consistent with the RNA and protein data described in the Human Protein Atlas (Tissue expression MUC1 / EMA)
Positive control: Kidney: Distal tubuli and collecting ducts must show a strong cytoplasmic MUC1 staining while the staining should be at least moderate in the parietal and visceral sheets of the Bowman’s capsule and largely absent in proximal tubuli.
Negative control: Colon: MUC1 staining should be very weak or absent in colonic epithelium.
Staining Pattern in Relevant Tumor Types
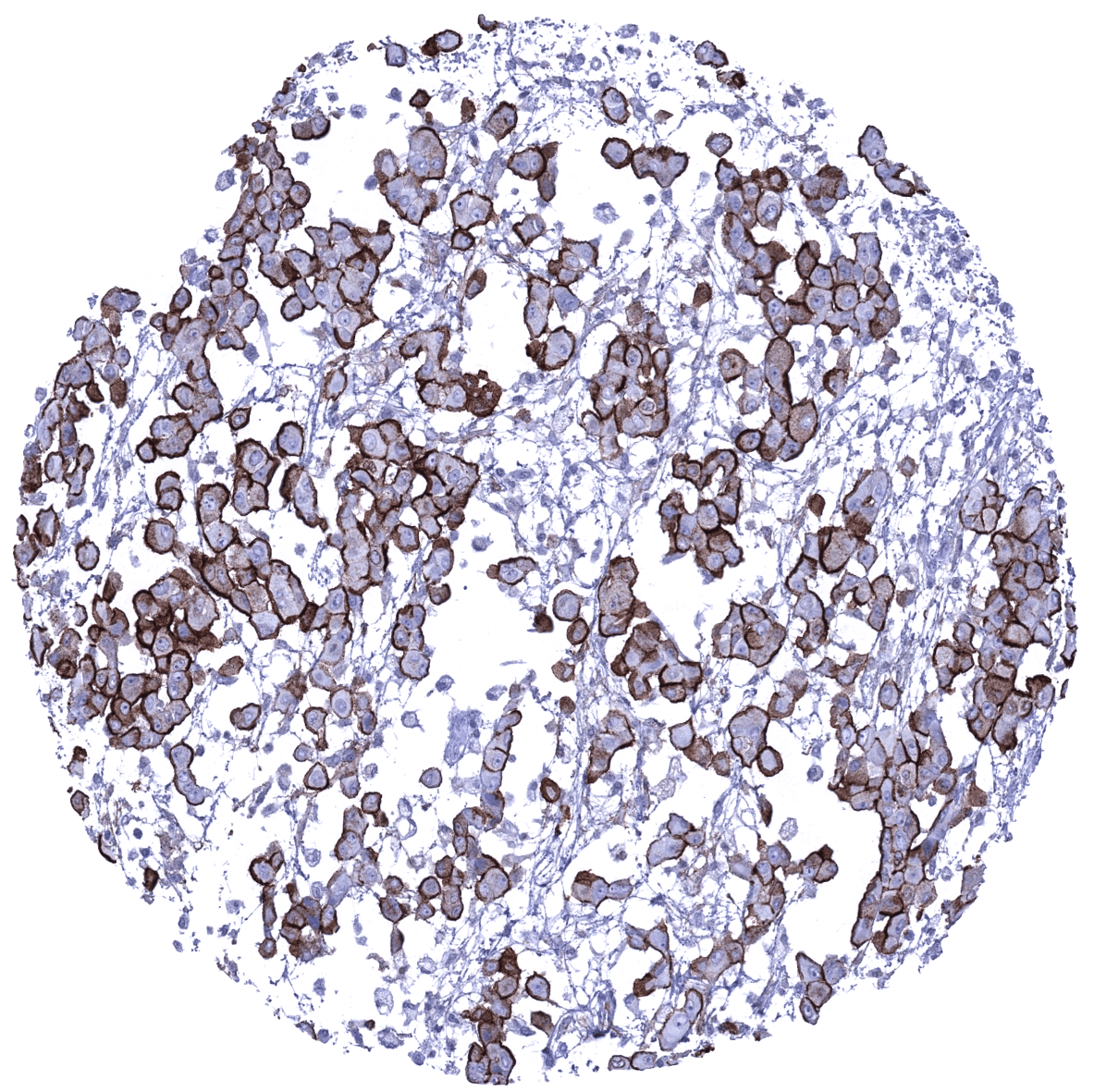
A variable level of MUC1 expression occurs in a large variety of adenocarcinomas and squamous cell carcinomas as well as in urothelial and renal neoplasms. In well-differentiated adenocarcinomas, the staining is often limited or focused to apical cell membranes while the staining is cytoplasmic with loss of staining polarity in less differentiated tumors. MUC1 positivity is frequent but less common in neuroendocrine and endocrine tumors, as well as in adenocarcinomas of the prostate. MUC1 immunostaining is rather rare in adrenocortical tumors, seminoma, and basal cell carcinoma. Among non-epithelial tumors, MUC1 may be found in ependymoma, meningioma, glial tumors, chordoma, perineurioma, solitary fibrous tumor, as well as in epithelioid and synovial sarcoma. In malignant mesothelioma, MUC1 is mainly seen on membranes of epithelioid cells and less commonly in the cytoplasm. MUC1 immunostaining can occasionally also occur in lymphomas including anaplastic large cell lymphoma, diffuse large B-cell lymphoma, plasma cell neoplasms, T-cell neoplasms, and nodular lymphocyte predominant Hodgkin’s lymphoma (L&H cells). MUC1 is very rarely or even never found in malignant melanoma or sex-cord stromal tumors.
The TCGA findings on MUC1 / EMA RNA expression in different tumor categories have been summarized in the Human Protein Atlas.
Compatibility of Antibodies
No data available at the moment
Protocol Recommendations
IHC users have different preferences on how the stains should look like. Some prefer high staining intensity of the target stain and even accept some background. Others favor absolute specificity and lighter target stains. Factors that invariably lead to more intense staining include higher concentration of the antibody and visualization tools, longer incubation time, higher temperature during incubation, higher temperature and longer duration of the heat induced epitope retrieval (slide pretreatment). The impact of the pH during slide pretreatment has variable effects and depends on the antibody and the target protein.
All images and data shown here and in our image galleries are obtained by the manual protocol described below. Other protocols resulting in equivalent staining are described as well.
Manual protocol
Freshly cut sections should be used (less than 10 days between cutting and staining). Heat-induced antigen retrieval for 5 minutes in an autoclave at 121°C in pH 7,8 Target Retrieval Solution buffer. Apply MSVA-672R at a dilution of 1:100 at 37°C for 60 minutes. Visualization of bound antibody by the EnVision Kit (Dako, Agilent) according to the manufacturer’s directions.
Impact of pH
MSVA-672R results in strongest staining if pH9,0 is used for slide pretreatment. pH7,8 & pH6 is also acceptable without resulting in a significant reduction of sensitivity.
Potential Research Applications
- A comprehensive study analyzing MUC1 expression in various tumor entities would be helpful to assess the diagnostic significance of MUC1 IHC.
- MUC1 is a potential therapeutic that can potentially be utilized for various treatment modalities.
- The signaling role of MUC1 is incompletely understood.
Evidence for Antibody Specificity in IHC
There are two ways how the specificity of antibodies can be documented for immunohistochemistry on formalin fixed tissues. These are: 1. comparison with a second independent method for target expression measurement across a large number of different tissue types (orthogonal strategy), and 2. Comparison with one or several independent antibodies for the same target and showing that all positive staining results are also seen with other antibodies for the same target (independent antibody strategy).
Orthogonal validation: For the antibody MSVA-672R specificity is suggested by the good concordance of the immunostaining data with data from three independent RNA screening studies, including the Human Protein Atlas (HPA) RNA-seq tissue dataset, the FANTOM5 project, and the Genotype-Tissue Expression (GTEx) project, which are all summarized in the Human Protein Atlas (Tissue expression MUC1). Immunostaining by using MSVA-672R was almost exclusively detected in organs with documented MUC1 RNA expression.
Comparison of antibodies: Further support for a specific staining reaction of MSVA-672R comes from the similarity of its staining pattern with stainings obtained by HPA007235 which are shown in the human protein atlas. Although the HPA007235 stainings are considerable less intense than those seen for MSVA-672R, they specifically confirm the staining patterns observed in:
- Kidney
- Urothelium
- Fallopian tube
- Endocervix
- Breast
- Stomach
- Colon (absence of staining)
- Gallbladder
- Pancreas
- Liver