295,00 € – 1.245,00 €
Product details
Synonyms = R3C3, Nuclear receptor subfamily 3 group C member 3, PGR, PR, PRA, PRB, Progesterone receptor form A, Progesterone receptor form B
Antibody type = Recombinant Rabbit monoclonal / IgG
Clone = MSVA-570R
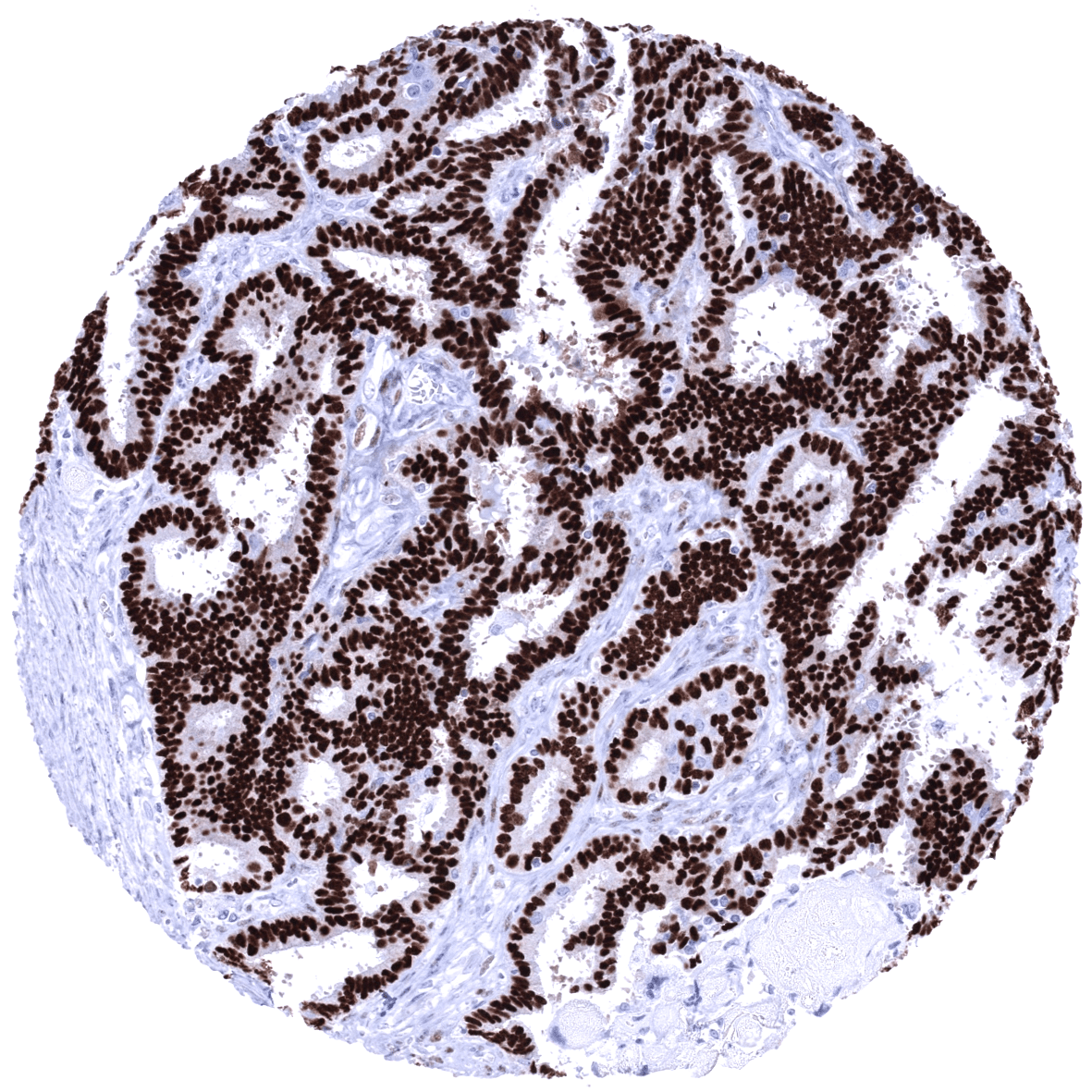
Positive control = Uterine cervix: almost all columnar epithelial cells, basal squamous epithelial cells and most of the stromal cells must show a strong nuclear staining with only minimal cytoplasmic staining.
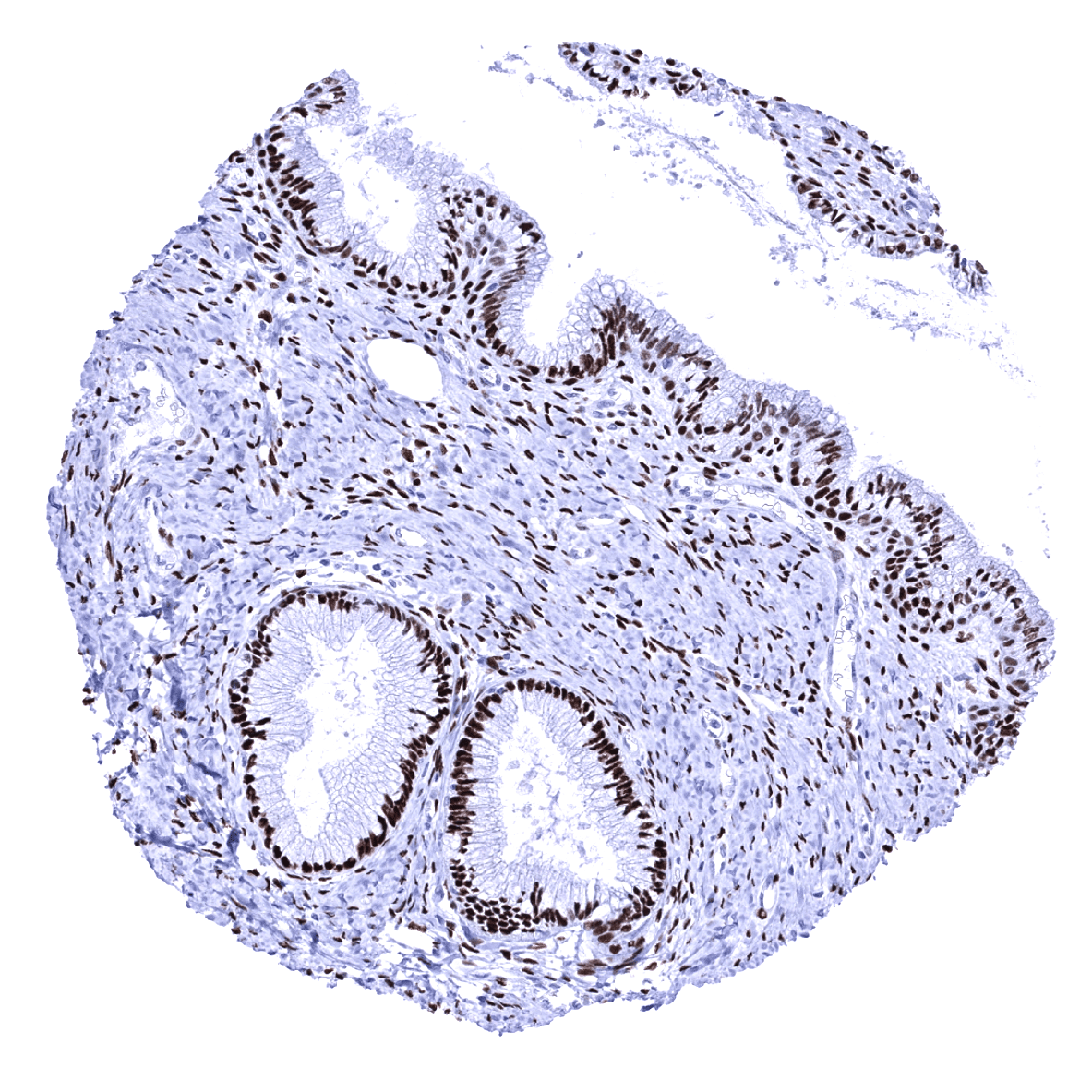
Negative control = Tonsil: PR immunostaining should be absent in all epithelial and non-epithelial cells.
Cellular localization = Nucleus
Reactivity = Human
Application = Immunohistochemistry
Dilution = 1:50
Intended Use = Research Use Only
Relevance of Antibody
Progesterone Receptor is expressed in progesterone dependent cell types.
Biology Behind
The progesterone receptor (PR), is a nuclear receptor protein coded by the PGR gene residing on chromosome 11q22. It is activated by the steroid hormone progesterone. In the absence of progesterone its carboxyl terminal inhibits transcription of target genes. After binding to progesterone, a structural change of the PR protein terminates the inhibitory action, the protein dimerizes, enters the nucleus, binds to DNA and induces transcription of target genes. Progesterone antagonists prevent the structural reconfiguration. Progesterone and its receptor are key elements of female reproduction. In breast development, progesterone is involved in the formation of lobular-alveolar units. In human endometrium, progesterone directs glandular differentiation, stromal proliferation and development of decidual cells. PR shares considerable sequence homology with the estrogen receptor (ER) in the DNA-binding central domain. The presence of a functional ER is required for PR synthesis in the cell. PR exists in two isoforms, PR-A and PR-B, which are often co-expressed in human tissues. They are transcribed from two different promoters of the PGR gene. The two PR isoforms are identical except that PR-A lacks 164 amino acids contained at the N-terminal end of PR-B. To some extent, the two isoforms have antagonistic functions. Predominant expression of one isoform can occur in some tissues under specific circumstances. PR-A is the major isoform in the uterine stroma, and PR-B is the predominant isoform in the endometrial glands. Normal human breast expresses PR-A and PR-B to equal extent.
Staining Pattern in Normal Tissues
Progesterone Receptor staining pattern in Normal Tissues with antibody MSVA-570R (images are shown in our “Normal Tissue Gallery”)
| Brain | Cerebrum | Negative. |
| Cerebellum | Negative. | |
| Endocrine Tissues | Thyroid | Negative. |
| Parathyroid | Negative. | |
| Adrenal gland | Weak to moderate PR staining of a variable fraction of adrenocortical cells (not in all samples). | |
| Pituitary gland | Weak to moderate PR staining of a variable number of epithelial cells in the adenohypophysis. Staining is absent in the neurohypophysis. | |
| Respiratory system | Respiratory epithelium | Negative. |
| Lung | Negative. | |
| Gastrointestinal Tract | Salivary glands | Weak to moderate PR positivity of some cells. |
| Esophagus | Weak to moderate PR positivity of some muscular cells in the muscular wall. | |
| Stomach | Negative. | |
| Duodenum | Weak to moderate PR positivity of some cells in Brunner glands. | |
| Small intestine | Weak to moderate PR positivity of some muscular cells in the muscular wall. | |
| Appendix | Negative. | |
| Colon | Negative. | |
| Rectum | Negative. | |
| Liver | Negative. | |
| Gallbladder | Negative. | |
| Pancreas | Weak to moderate to strong PR staining of a large fraction of islet cells. | |
| Genitourinary | Kidney | Weak to moderate PR staining in subsets of glomerular, tubular and stromal cells. |
| Urothelium | Weak to moderate to strong PR staining in stroma cells of the urinary bladder and the pyelon. The urothelium is negative. | |
| Male genital | Prostate | Moderate to strong PR staining of stromal cells. |
| Seminal vesicles | Moderate to strong PR staining of stromal cells. | |
| Testis | Negative. | |
| Epididymis | Weak to moderate PR staining of epithelial cells of the cauda. | |
| Female genital | Breast | Moderate to strong PR staining of a fraction of luminal epithelial cells. |
| Uterus, myometrium | Strong PR staining of muscular cells. | |
| Uterus, ectocervix | Strong PR staining of stromal cells and basal squamous epithelial cells. | |
| Uterus endocervix | Strong PR staining of epithelial and stromal cells. | |
| Uterus, endometrium | Strong PR staining of epithelial, decidual, and stromal cells. | |
| Fallopian Tube | Strong PR staining of epithelial and stromal cells. | |
| Ovary | Strong PR staining of stromal cells and corpus luteum. | |
| Placenta early | Negative. | |
| Placenta mature | Negative. | |
| Amnion | Negative. | |
| Chorion | Negative. | |
| Skin | Epidermis | Negative. |
| Sebaceous glands | Negative. | |
| Muscle/connective tissue | Heart muscle | Negative. |
| Skeletal muscle | Negative. | |
| Smooth muscle | Negative. | |
| Vessel walls | Moderate to strong PR staining of smooth muscle cells in the media of the aorta. | |
| Fat | Negative. | |
| Stroma | PR staining can be found in some stroma cells of various organs. | |
| Endothelium | Negative. | |
| Bone marrow/ lymphoid tissue | Bone marrow | Negative. |
| Lymph node | Negative. | |
| Spleen | Negative. | |
| Thymus | Negative. | |
| Tonsil | Negative. | |
| Remarks | PR staining is nuclear. |
These findings are largely consistent with the RNA and protein data described in the Human Protein Atlas (Tissue expression Progesterone Receptor)
Positive control: Uterine cervix: almost all columnar epithelial cells, basal squamous epithelial cells and most of the stromal cells must show a strong nuclear staining with only minimal cytoplasmic staining.
Negative control: Tonsil: PR immunostaining should be absent in all epithelial and non-epithelial cells.
Staining Pattern in Relevant Tumor Types
The TCGA database on RNA expression in cancer has described the highest levels of PR expression in breast and endometrial cancer followed by ovarian and cervical cancer. Most other important tumor entities are described to be usually “PR negative”.
The TCGA findings on Progesterone Receptor RNA expression in different tumor categories have been summarized in the Human Protein Atlas.
Compatibility of Antibodies
Progesterone receptor (PR) (MSVA-570R) publication summary
Relevant publication: Viehweger et al. “Diagnostic and Prognostic Impact of Progesterone Receptor Immunohistochemistry: A Study Evaluating More Than 16,000 Tumors”. Pathol (Amst). 2022 Aug 8;2022:6412148. PMID: 35992051
A total of 16,445 tumors were successfully analyzed from 147 different tumor categories by using the following protocol: Heat-induced antigen retrieval for 5 minutes in an autoclave at 121°C in pH7,8 Target Retrieval Solution buffer. MSVA-570R at a dilution of 1:50 at 37°C for 60 minutes. Visualization of bound antibody by the EnVision Kit (Dako, Agilent). This protocol was also used for all stainings depicted in our tumor and normal tissue galleries.
In this study, at least one progesterone receptor (PR) positive case was seen in 55 (37.4%) of 147 tumor categories and 31 (21%) tumor categories included at least one case with strong positivity. PR immunostaining was detected in 57.4% of breast tumors, 28.6% of other gynecological tumors, and 1.8% of non-gynecological and non-mammary tumors. The highest PR positivity rates among non-gynecological tumors occurred in neuroendocrine tumors (54.3%) and neuroendocrine carcinomas (35.7%) of the pancreas, testicular Leydig cell tumor (36.7%), medullary thyroid carcinoma (20.4%), small cell neuroendocrine carcinomas of the prostate (16.7%) and the lung (12.5%), angiomyolipoma (12.5%), adrenal cortical carcinoma (11.5%), follicular thyroid carcinoma (11.3%), and papillary thyroid carcinoma (10.6%). The distribution of positive PR staining results is shown in an “organ-systematic” and in a “ranking order” figure below (images based on data from Viehweger et al.). Results on possible associations with histopathological and clinical parameters of tumor aggressiveness are also summarized below (table based on data from Viehweger et al.).
Authors conclusions on diagnostic utility of PR immunohistochemistry with respect to the distinction of different tumor entities (Viehweger et al.):
- Identification of PR positive breast cancer (likely to respond to hormonal therapy).
- In case of tumor masses of unknown origin, PR positivity argues for a cancer origin from the breast or from other gynecological organs (many exceptions occur).
- Distinction of neuroendocrine tumors or carcinomas derived from the pancreas (often PR positive) from neuroendocrine neoplasms from other sites of origin (often PR negative).
Authors conclusions on prognostic/predictive role of PR expression (Viehweger et al.):
- PR positivity argues for a favorable prognosis in breast cancer patients.
- Low PR expression is linked to nodal metastasis in endometrioid endometrium carcinoma.
Figure 1. Progesterone Receptor staining in cancer (“organ-systematic”; according to Viehweger et al.)
Figure 2. Progesterone Receptor staining in cancer (“ranking list”; according to Viehweger et al.)
Protocol Recommendations
IHC users have different preferences on how the stains should look like. Some prefer high staining intensity of the target stain and even accept some background. Others favor absolute specificity and lighter target stains. Factors that invariably lead to more intense staining include higher concentration of the antibody and visualization tools, longer incubation time, higher temperature during incubation, higher temperature and longer duration of the heat induced epitope retrieval (slide pretreatment). The impact of the pH during slide pretreatment has variable effects and depends on the antibody and the target protein.
All images and data shown here and in our image galleries are obtained by the manual protocol described below. Other protocols resulting in equivalent staining are described as well.
Manual protocol
Freshly cut sections should be used (less than 10 days between cutting and staining). Heat-induced antigen retrieval for 5 minutes in an autoclave at 121°C in pH 7,8 Target Retrieval Solution buffer. Apply MSVA-570R at a dilution of 1:50 at 37°C for 60 minutes. Visualization of bound antibody by the EnVision Kit (Dako, Agilent) according to the manufacturer’s directions.
Agilent / Dako – Autostainer Link 48
Pretreatment in PT-Link for 30 minutes at 95°C (pH high); FLEX peroxidase blocking for 5 minutes (room temperature), MSVA-570R 1:50 for 20 minutes (room temperature), FLEX+ mouse/rabbit (LINKER) for 15 minutes (room temperature), horseradish peroxidase (HRP) for 20 minutes (room temperature), FLEX DAB+Sub-Chromo for 10 minutes (room temperature), FLEX hematoxylin for 5 minutes (room temperature).
These images reflect stainings by the protocol described above. It is of note that a comparable staining result can also be obtained by different protocols. In general, a longer pretreatment, a longer incubation time of the primary antibody, a higher antibody concentration, and a longer incubation time of FLEX+LINKER result in stronger staining, potentially at the cost of more background staining. Modifications of the protocol with a strengthening effect on staining intensity in combination with changes of other parameters that result in lower staining intensity can result in a comparable result as shown above.
Leica – BOND RX
Dewax at 72°C for 30 seconds; Pretreatment in Bond Epitope Retrieval Solution (ER2 – EDTA pH9) for 20 minutes at 100°C; Peroxidase blocking for 5 minutes (room temperature), MSVA-570R 1:100 for 15 minutes (room temperature), Post primary (rabbit anti mouse) for 8 minutes (room temperature), Polymer (goat anti rabbit) for 8 minutes (room temperature), mixed DAB refine for 10 minutes (room temperature), hematoxylin for 5 minutes (room temperature).
These images reflect stainings by the protocol described above. It is of note that a comparable staining result can also be obtained by different protocols. In general, a longer pretreatment, a longer incubation time of the primary antibody, a higher antibody concentration, a higher temperature during incubation, and a longer incubation time of Post primary and or the Polymer result in stronger staining, potentially at the cost of more background staining. Modifications of the protocol with a strengthening effect on staining intensity in combination with changes of other parameters that result in lower staining intensity can result in a comparable result as shown above.
Roche – Ventana Discovery ULTRA
Pretreatment for 64 minutes at 100°C (pH 8,4); CM peroxidase blocking for 12 minutes (room temperature), MSVA-570R 1:50 for 20 minutes at 36°C, secondary antibody (anti-rabbit HQ) for 12 minutes at 36°C, anti-HQ HRP for 12 minutes at room temperature, DAB at room temperature, hematoxylin II at room temperature for 8 minutes, bluing reagent at room temperature for 4 minutes.
These images depict staining results obtained by the protocol described above. It is of note, that the Ventana machines generally require higher antibody concentrations than other commonly used autostainers because the antibodies are automatically diluted during the procedure. Various other protocols can result in an identical result as shown above. A longer pretreatment, a longer incubation time of the primary antibody, a higher antibody concentration, a higher temperature during incubation, and a longer incubation time of secondary antibody and or the anti-HQ HRP result in stronger staining, potentially at the cost of more background staining.
Potential Research Applications
- The diagnostic utility of PR expression analysis should be investigated in a large cohort of tumors from different entities.
- The clinical/biological significance of the rare ER-/PR+ breast cancers is unclear.
- Much is still unknown on the site-specific role of PR in various different tissues.