295,00 € – 895,00 €
Product details
Synonyms = ASP4, Aspartyl protease 4, KAP, Kidney derived aspartic protease like protein (Kdap), NAP1, NAPA, Napsa, napsin A aspartic peptidase, Pronapsin A, SNAPA
Antibody type = Recombinant Rabbit monoclonal / IgG
Clone = MSVA-112R
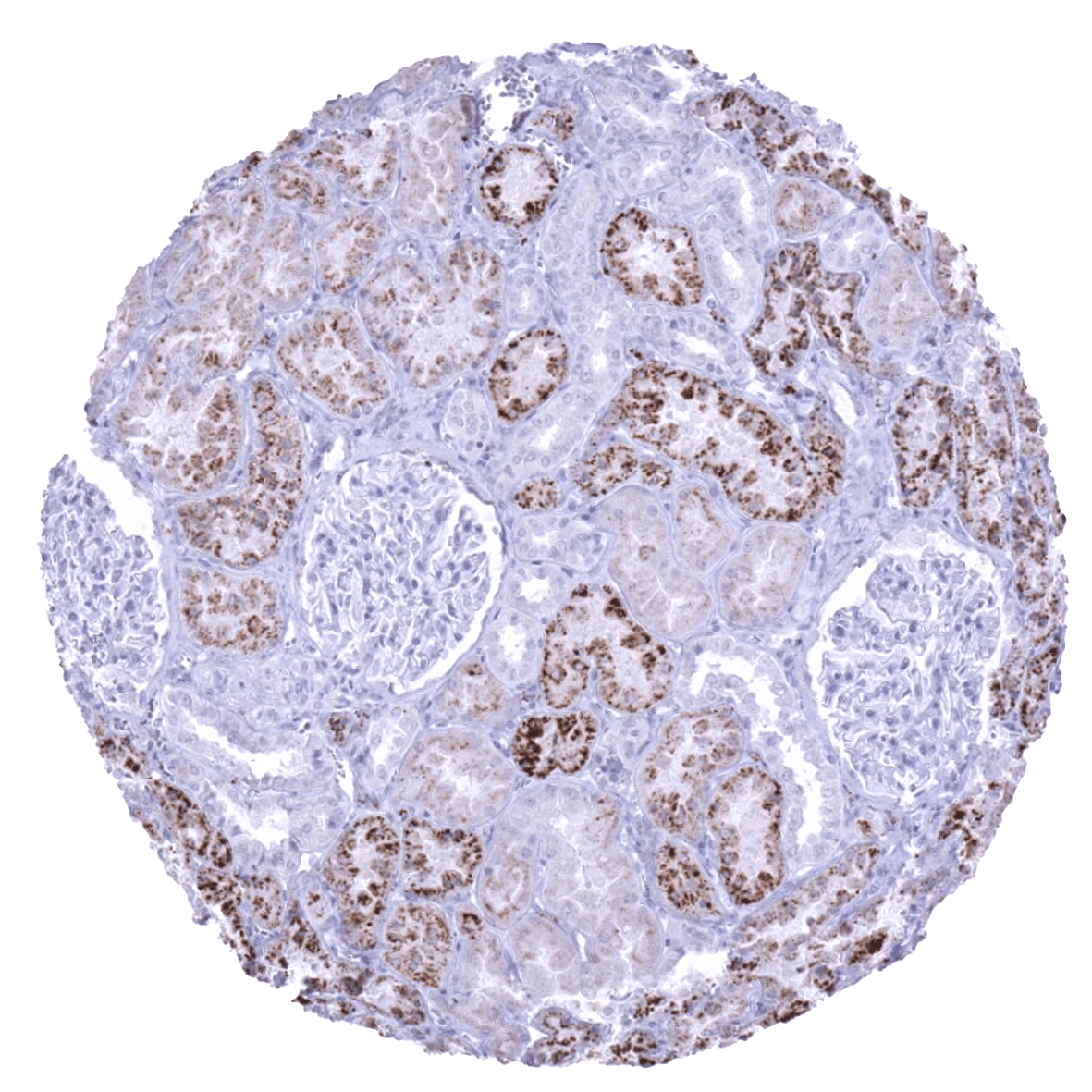
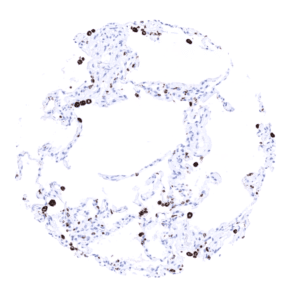
Positive control = Kidney: an at least moderate granular cytoplasmic staining should be seen in proximal tubule cells
Negative control = Colon: staining should be absent in epithelial and other cells of the lamina propria.
Cellular localization = Cytoplasmic
Reactivity = Human
Application = Immunohistochemistry
Dilution = 1:100 – 1:200
Intended Use = Research Use Only
Relevance of Antibody
Biology Behind
Novel aspartic proteinase of the pepsin family A (Napsin A, TAO1/TAO2) belongs to the peptidase A1 family, together with Cathepsin E, renin, and pepsin. Napsin A is a proteinase, that cleaves proteins and peptides to produce mature or active forms of these molecules. Napsin A is known to be expressed in type II pneumocytes, intra-alveolar macrophages, and in renal tubules. Physiologically, Napsin A is involved in the maturation of prosurfactant protein B in type II pneumocytes, phagocytosis by macrophages, and protein catabolism in renal cells. In the lung, Napsin A is regulated by the thyroid transcription factor 1 (TTF1). Napsin A expression is limited to few cancer types. Napsin A immunohistochemistry is therefore highly useful for distinction of different tumor types in the lung and in the ovary as well as for assessing tumors of unknown origin.[1]
[1] Weidemann et al. “Napsin A Expression in Human Tumors and Normal Tissues” Pathology & Oncology Research 2021; 27: 613099
Staining Pattern in Normal Tissues
Napsin staining pattern in Normal Tissues with antibody MSVA-112R (images are shown in our “Normal Tissue Gallery”)
| Brain | Cerebrum | Negative. |
| Cerebellum | Negative. | |
| Endocrine Tissues | Thyroid | Negative. |
| Parathyroid | Negative. | |
| Adrenal gland | Negative. | |
| Pituitary gland | Negative. | |
| Respiratory system | Respiratory epithelium | Negative. |
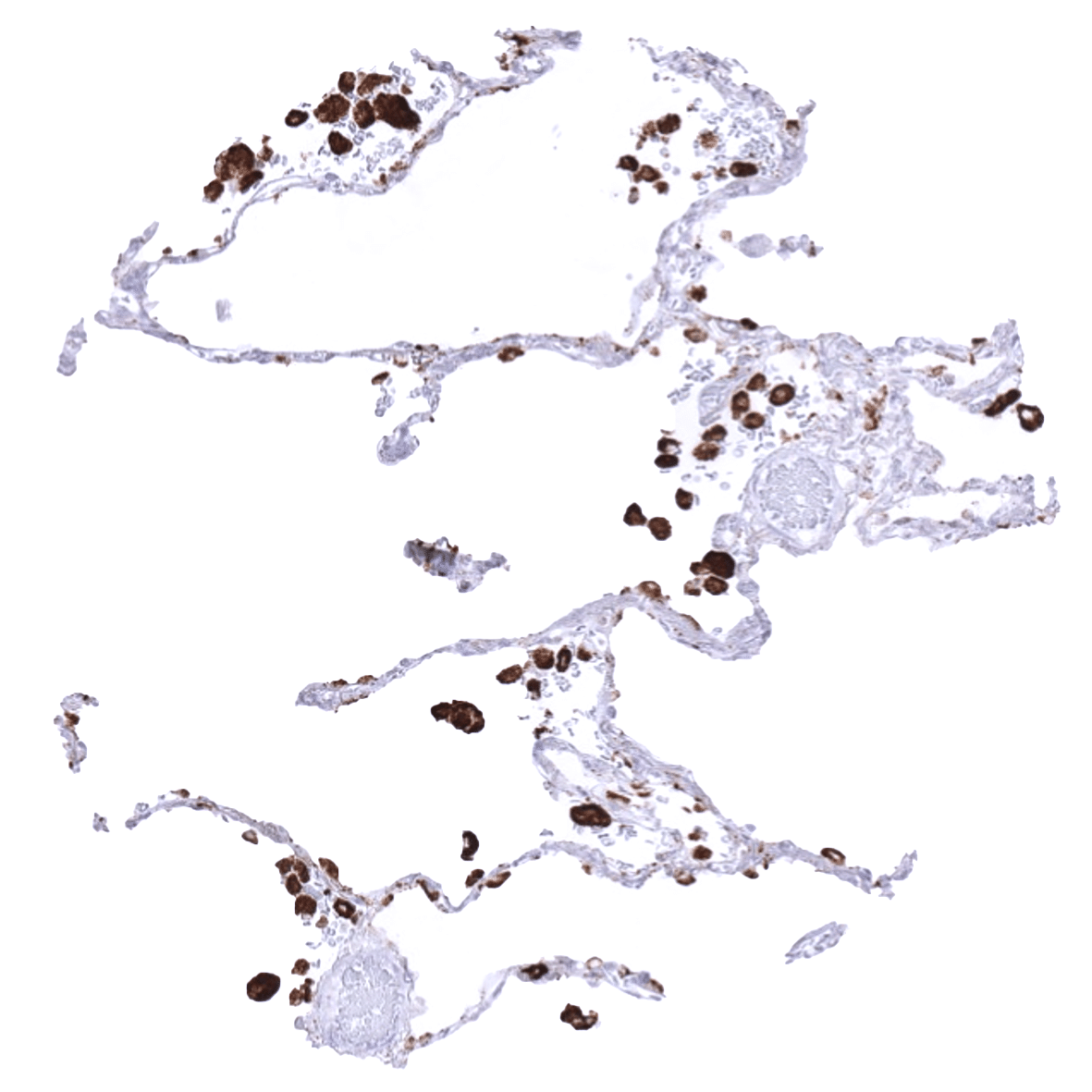
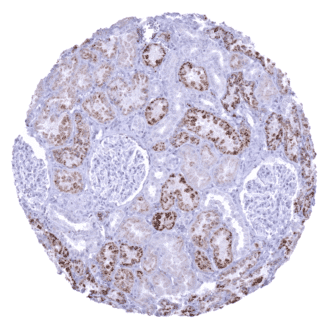
| Lung | Very strong cytoplasmic Napsin A staining in type II pneumocytes and in alveolar macrophages. | |
| Gastrointestinal Tract | Salivary glands | Negative. |
| Esophagus | Negative. | |
| Stomach | Negative. | |
| Colon | Negative. | |
| Duodenum | Negative. | |
| Rectum | Negative. | |
| Small intestine | Negative. | |
| Liver | Negative. | |
| Gallbladder | Negative. | |
| Pancreas | Negative. | |
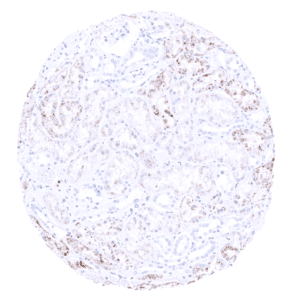
| Genitourinary | Kidney | Napsin A staining is variable and ranges from weak to strong. Proximal tubuli stain more strongly than distal tubuli. Some collecting ducts also stain positive. |
| Urothelium | Negative. | |
| Male genital | Prostate | Negative. |
| Seminal vesicles | Negative. | |
| Testis | Negative. | |
| Epididymis | Moderate to strong Napsin A positivity occurs at the luminal pole of epithelial cells of the cauda while the corpus epididymis is Napsin ANegative. | |
| Female genital | Breast | Negative. |
| Uterus, myometrium | Negative. | |
| Uterus, ectocervix | Negative. | |
| Uterus endocervix | Negative. | |
| Uterus, endometrium | Occasional staining can occur in some endometrial glands in some samples. | |
| Fallopian Tube | Negative. | |
| Ovary | Negative. | |
| Placenta early | Negative. | |
| Placenta mature | Negative. | |
| Amnion | Negative. | |
| Chorion | Negative. | |
| Skin | Epidermis | Negative. |
| Sebaceous glands | Negative. | |
| Muscle/connective tissue | Heart muscle | Negative. |
| Skeletal muscle | Negative. | |
| Smooth muscle | Negative. | |
| Fat | Negative. | |
| Stroma | Negative. | |
| Endothelium | Negative. | |
| Bone marrow/lymphoid | Bone marrow | Negative. |
| Lymph node | Negative. | |
| Spleen | Negative. | |
| Thymus | Negative. | |
| Tonsil | Negative. | |
| Remarks |
These findings are largely consistent with the RNA and protein data described in the Human Protein Atlas (Tissue expression Napsin A)
Suggested positive tissue control: Kidney is better suited as a control tissue than lung because even insensitive protocols may detect the highly expressed Napsin A in pneumocytes and alveolar macrophages of the normal lung. In kidney, all epithelial cells of the proximal tubules must show an at least moderate cytoplasmic immunostaining.
Suggested negative tissue control: Colon: Napsin A staining should be absent in normal epithelial cells and macrophages in the lamina propria.
Staining Pattern in Relevant Tumor Types
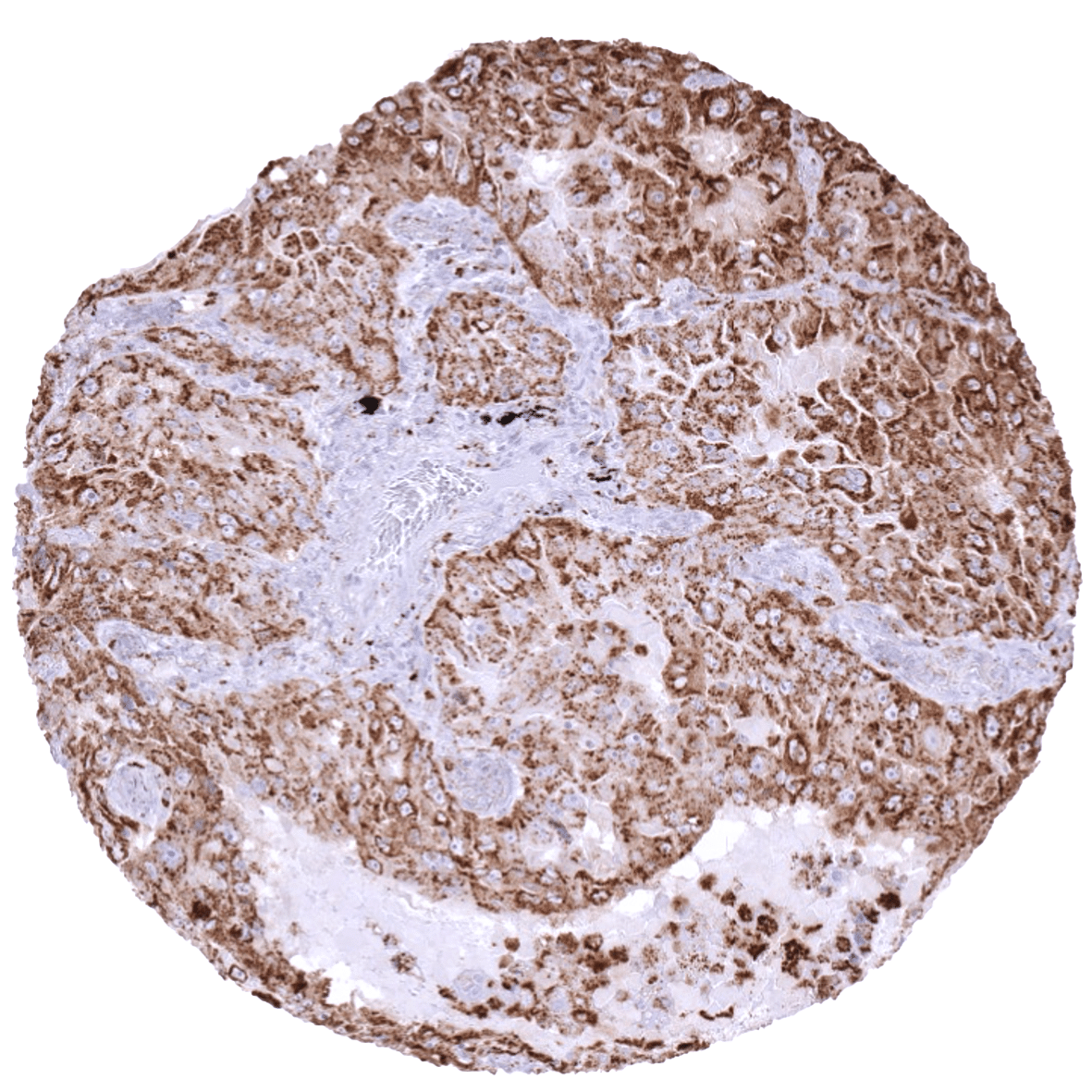
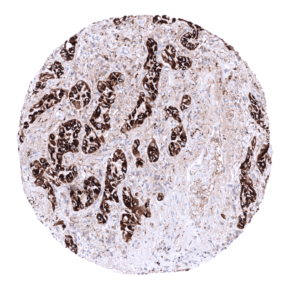
The most commonly Napsin A positive cancer types include: adenocarcinoma of the lung (approx. 85% positive), clear cell adenocarcinoma of the ovary (70%) and the endometrium (40%), papillary renal cell carcinoma (40%), small cell carcinoma of the lung (20%), endometroid serous carcinoma (10%), papillary thyroid carcinoma (10%) and clear cell renal cell carcinoma (10%).
The TCGA findings on Napsin A RNA expression in different tumor categories have been summarized in the Human Protein Atlas.
Compatibility of Antibodies
Napsin A (MSVA-112R) publication summary
Relevant publication: Weidemann et al. “Napsin A Expression in Human Tumors and Normal Tissues” Published in Pathology & Oncology Research 2021; 27: 613099
A total of 11957 tumors were analyzed from 115 different tumor categories by using the following protocol: Heat-induced antigen retrieval for 5 minutes in an autoclave at 121°C in pH7,8 Target Retrieval Solution buffer. MSVA-112R at a dilution of 1:200 at 37°C for 60 minutes. Visualization of bound antibody by the EnVision Kit (Dako, Agilent). This protocol was also used for all stainings depicted in our tumor and normal tissue galleries.
At least one case with a positive Napsin A immunostaining was seen in 16 (13,9%) and at least one case with a strong Napsin A immunostaining was seen in 6 (5,2%) of 115 tumor categories. The distribution of positive staining results is shown “organ-systematic” and in a “ranking order” figure below (images based on data from Weidemann et al). Results on possible associations with histopathological and clinical parameters of tumor aggressiveness in renal cell carcinomas are also summarized below (table based on data from Weidemann et al). Of note, for this analysis a higher antibody concentration had been selected.
Authors conclusions on diagnostic utility with respect to the distinction of benign versus malignant (Weidemann et al):
- none
Authors conclusions on diagnostic utility with respect to the distinction of different tumor entities (Weidemann et al):
- A strong role of Napsin A in the difficult distinction of adenocarcinoma and squamous cell carcinoma in the lung is strongly supported by our Napsin positivity of 85.6% in 198 adenocarcinomas, while none of our 79 squamous cell carcinomas were found positive.
- It is of note that other investigators have reported Napsin A positivity in up to 10% of pulmonary squamous cell carcinomas. Entrapped normal lung tissue with Napsin A positive hyperplastic pneumocytes or Napsin A positive intra-alveolar macrophages could be the cause for such findings.
- The limitation of Napsin A immunostaining to few cancer types makes Napsin A highly useful marker for assessing the site of origin of cancers. It is a potential pitfall, however, that several cancer types, that often metastasize to the lung belong to the exclusive group of potentially Napsin A positive cancers, such as renal cell carcinoma, urothelial cancer, colorectal carcinoma and clear cell carcinomas of the ovary and the endometrium. Several reports have indeed described that metastatic renal cell carcinomas were misdiagnosed as a primary adenocarcinoma of the lung on the basis of Napsin A positivity.
- In case of an ovarian cancer, Napsin A immunostaining is a strong argument for a celar cell carcinoma.
Authors conclusions on prognostic/predictive role of Napsin A expression (Weidemann et al.):
- Low expression of Napsin A was linked to unfavorable tumor features and poor prognosis in papillary and clear cell renal cell carcinomas.
Data from the publication: “Napsin A Expression in Human Tumors and Normal Tissues”. Published by Weidemann et al. in Pathology & Oncology Research 2021; 27: 613099
Summarized in own graphics:
1. Napsin A staining in tumors “organ-specific” with antibody MSVA-112R.
2. Napsin A staining in tumors “ranking order” by positivity with antibody MSVA-112R.
Protocol Recommendations
IHC users have different preferences on how the stains should look like. Some prefer high staining intensity of the target stain and even accept some background. Others favor absolute specificity and lighter target stains. Factors that invariably lead to more intense staining include higher concentration of the antibody and visualization tools, longer incubation time, higher temperature during incubation, higher temperature and longer duration of the heat induced epitope retrieval (slide pretreatment). The impact of the pH during slide pretreatment has variable effects and depends on the antibody and the target protein.
All images and data shown here and in our image galleries are obtained by the manual protocol described below. Other protocols resulting in equivalent staining are described as well.
Manual protocol
Freshly cut sections should be used (less than 10 days between cutting and staining). Heat-induced antigen retrieval for 5 minutes in an autoclave at 121°C in pH 7,8 Target Retrieval Solution buffer. Apply MSVA-112R at a dilution of 1:150 at 37°C for 60 minutes. Visualization of bound antibody by the EnVision Kit (Dako, Agilent) according to the manufacturer’s directions.
Agilent / Dako – Omnis
Unmasking IHC EnV FLEX TRS High pH 97°C ; FLEX peroxidase blocking for 3 minutes (32°C), MSVA-112R 1:600 for 30 minutes at 32°C, FLEX+ mouse/rabbit (LINKER) for 10 minutes at 32°C, horseradish peroxidase (HRP) for 30 minutes (32°C), FLEX DAB+Sub-Chromo for 5 minutes (32°C), FLEX hematoxylin for 5 minutes (room temperature).
These images reflect stainings by the protocol described above. It is of note that a comparable staining result can also be obtained by different protocols. In general, a longer pretreatment, a longer incubation time of the primary antibody, a higher antibody concentration, and a longer incubation time of FLEX+LINKER result in stronger staining, potentially at the cost of more background staining. Modifications of the protocol with a strengthening effect on staining intensity in combination with changes of other parameters that result in lower staining intensity can result in a comparable result as shown above.
Agilent / Dako – Autostainer Link 48
Pretreatment in PT-Link for 30 minutes at 95°C (pH high); FLEX peroxidase blocking for 5 minutes (room temperature), MSVA-112R 1:150 for 20 minutes (room temperature), FLEX+ mouse/rabbit (LINKER) for 15 minutes (room temperature), horseradish peroxidase (HRP) for 20 minutes (room temperature), FLEX DAB+Sub-Chromo for 10 minutes (room temperature), FLEX hematoxylin for 5 minutes (room temperature).
These images reflect stainings by the protocol described above. It is of note that a comparable staining result can also be obtained by different protocols. In general, a longer pretreatment, a longer incubation time of the primary antibody, a higher antibody concentration, and a longer incubation time of FLEX+LINKER result in stronger staining, potentially at the cost of more background staining. Modifications of the protocol with a strengthening effect on staining intensity in combination with changes of other parameters that result in lower staining intensity can result in a comparable result as shown above.
Leica – BOND RX
Dewax at 72°C for 30 seconds; Pretreatment in Bond Epitope Retrieval Solution (ER2 – EDTA pH9) for 20 minutes at 100°C; Peroxidase blocking for 5 minutes (room temperature), MSVA-112R 1:150 for 15 minutes (room temperature), Post primary (rabbit anti mouse) for 8 minutes (room temperature), Polymer (goat anti rabbit) for 8 minutes (room temperature), mixed DAB refine for 10 minutes (room temperature), hematoxylin for 5 minutes (room temperature).
These images reflect stainings by the protocol described above. It is of note that a comparable staining result can also be obtained by different protocols. In general, a longer pretreatment, a longer incubation time of the primary antibody, a higher antibody concentration, a higher temperature during incubation, and a longer incubation time of Post primary and or the Polymer result in stronger staining, potentially at the cost of more background staining. Modifications of the protocol with a strengthening effect on staining intensity in combination with changes of other parameters that result in lower staining intensity can result in a comparable result as shown above.
Roche – Ventana Discovery ULTRA
Pretreatment for 64 minutes at 100°C (pH 8,4); CM peroxidase blocking for 12 minutes (room temperature), MSVA-112R 1:200 for 20 minutes at 36°C, secondary antibody (anti-rabbit HQ) for 12 minutes at 36°C, anti-HQ HRP for 12 minutes at room temperature, DAB at room temperature, hematoxylin II at room temperature for 8 minutes, bluing reagent at room temperature for 4 minutes.
These images depict staining results obtained by the protocol described above. It is of note, that the Ventana machines generally require higher antibody concentrations than other commonly used autostainers because the antibodies are automatically diluted during the procedure. Various other protocols can result in an identical result as shown above. A longer pretreatment, a longer incubation time of the primary antibody, a higher antibody concentration, a higher temperature during incubation, and a longer incubation time of secondary antibody and or the anti-HQ HRP result in stronger staining, potentially at the cost of more background staining.
Potential Research Applications
- A comprehensive study analyzing Napsin-A expression in various different tumor entities would be helpful to assess the diagnostic significance of Napsin-A IHC.
- The clinical role of Napsin A expression levels in lung or renal cancers is unknown.
Evidence for Antibody Specificity in IHC
Specificity of MSVA-112R is documented by strong positive staining in cell types that are well documented to express Napsin A such as pneumocytes and alveolar macrophages in the lung, proximal tubuli in the kidney and epithelial cells in the epididymis. In addition Napsina A immunostaining was absent in all tissues known to not express Napsin A including tissues notorious for non-specific IHC background such as kidney, colonic mucosa, and epidermis.